Important Takeaways:
- The leader of Canada’s most populous province has followed through on a pledge to hike electricity prices for Americans in response to President Trump’s tariffs as residents of US border states New York, Minnesota and Michigan can expect to pay more for power.
- The Canadian province of Ontario raised electricity export prices by 25% for the three American states on Monday — marking a direct response to the escalating trade dispute between the two countries.
- Ontario Premier Doug Ford ordered the Independent Electricity System Operator, which oversees the province’s electricity market, to implement a $7-per-megawatt-per-hour fee on all power exports to the three states, Bloomberg News reported.
- Despite the aggressive stance, the actual impact on US consumers may be minimal.
- Electricity prices on US spot markets, where power is bought and sold in real-time, fluctuate based on supply and demand.
- With multiple sources available, American buyers are not obligated to purchase from Ontario, meaning they may be able to source cheaper electricity from alternative suppliers.
- New York imported about 4.4% of its total electricity from Canada in 2023, according to Bloomberg calculations using data from the state’s grid operator.
- Minnesota and Michigan relied on Canadian imports even less, according to the Midcontinent Independent System Operator (MISO), which manages the power grid across much of the Midwest.
- “In 2024, less than 1% of MISO’s total energy was supplied via Canadian imports and less than half of that came from Ontario”
Read the original article by clicking here.

Important Takeaways:
- A long-duration lake-effect snowstorm is continuing to pummel the Great Lakes region after dumping 3-5 feet of snow in cities from Michigan to New York that paralyzed travel as people tried to get home after the busy Thanksgiving holiday weekend.
- The impacts from the historic lake-effect snowstorm have been far-reaching, not only because of the sheer amount of snow that fell but also because of the intense snowfall rates reaching up to 4 inches per hour, which overwhelmed crews who were relentlessly working around the clock to remove the snow and ice from roads and highways such as the heavily traveled Interstate 90 from New York state to Ohio
- Travel is expected to remain treacherous in areas still impacted by bands of heavy snow coming off the Great Lakes. Drivers are being urged to stay off the roads if possible, significantly slow their speeds, and leave plenty of distance between vehicles to ensure the safety of people out and about on Monday.
- And it wasn’t just the snow that was making headlines over the weekend. The paralyzing lake-effect snowstorm also produced rare thundersnow and even waterspouts off the shores of Lake Erie.
- Winter weather alerts remain in effect across the region, including Lake-Effect Snow Warnings from Cleveland to southwestern New York that will remain in effect until at least Tuesday morning.
- Travel could again become dangerous on major roads and highways across the region, including I-90, I-86 and I-79, which could become nearly impassable. In the heaviest snow bands, visibility could drop to less than a quarter-mile, and strong winds could blow snow that has already fallen.
Read the original article by clicking here.

Important Takeaways:
- Largest fresh egg producer in U.S. finds bird flu in chickens at Texas and Michigan plants
- The largest producer of fresh eggs in the U.S. said Tuesday it had temporarily halted production at a Texas plant after bird flu was found in chickens, and officials said the virus had also been detected at a poultry facility in Michigan.
- In Texas, Ridgeland, Mississippi-based Cal-Maine Foods, Inc. said in a statement that approximately 1.6 million laying hens and 337,000 pullets, about 3.6% of its total flock, were destroyed after the infection, avian influenza, was found at the facility in Parmer County, Texas.
- The plant is on the Texas-New Mexico border in the Texas Panhandle about 85 miles southwest of Amarillo and about 370 miles northwest of Dallas.
- “The Company continues to work closely with federal, state and local government officials and focused industry groups to mitigate the risk of future outbreaks and effectively manage the response,” according to the statement. “Cal-Maine Foods is working to secure production from other facilities to minimize disruption to its customers.”
- The company said there is no known bird flu risk associated with eggs that are currently on the market and no eggs have been recalled. Eggs that are properly handled and cooked are safe to eat, according to the U.S. Department of Agriculture.
Read the original article by clicking here.

Important Takeaways:
- A previously deported illegal alien, identified as Brandon Ortiz-Vite, was arrested and charged with the murder of 25-year-old Ruby Garcia in Kent County, Michigan.
- The illegal from Mexico was charged with felony murder, open murder, carjacking, carrying a concealed weapon, and felony possession of a firearm for the March 22 incident.
- With the news of the arrest still so recent, Whitmer is taking heat for her program, which provides $500 per month for housing assistance to private homeowners who agree to take in migrants.
- Tudor Dixon, who ran for governor as a Republican in 2022, blasted Whitmer, saying that she is “enabling Joe Biden’s open border policies by handing out cash to anyone who will take in unvetted illegal immigrants, undoubtedly risking the safety of our neighborhoods and communities,”
- “After the murder of Ruby Garcia less than a week ago, Whitmer should immediately cancel this program and demand Biden secure the border for the good of Michigan citizens,” Dixon added
Read the original article by clicking here.

Important Takeaways:
- Extreme weather and severe thunderstorms swept through Michigan overnight Tuesday, spawning reports early Wednesday of damage, power outages, and three tornadoes near Grand Blanc, Marshall and Lawton.
- The storms illustrated Mother Nature’s power and volatility, as sunny blue skies and record-warm temperatures in the low 70s quickly gave way to tempests that downed trees and power lines and damaged homes, businesses and automobiles.
- …about 15,000 customers were without electricity.
- In Grand Blanc, radar showed a tornado touched down, causing serious damage to neighborhoods and potentially a General Motors facility, according to social media posts. The extent of it will become clearer in the daylight.
Read the original article by clicking here.

Important Takeaways:
- ‘Transnational gangs’ conduct ‘high-end burglaries’ in Oakland County, sheriff says
- Oakland County Sheriff Michael Bouchard called Friday for tighter border security as his office works with multiple agencies to intercept the efforts of “transnational gangs” involved in “high-end burglaries,” prowling across Oakland County and throughout the nation.
- The sheriff detailed at a press conference what officials have learned about the burglaries that have ravaged Michigan’s second most populous county, resulting in what Bouchard described as the loss of “hundreds and hundreds of thousands of dollars” worth of merchandise. He did not detail how many arrests have been made or other details authorities have complied in connection with incidents but said “there are specific threads” officials are aware of.
- “These are transnational gangs that are involved in this that come from South America, looking to do burglaries and violate our communities, not just in Oakland County but across America,” Bouchard said. “It’s criminality at its organized crime best in terms of that’s how it functions. They work together, and they’re here for a specific purpose.”
Read the original article by clicking here.

Important Takeaways:
- Michigan tornado leaves overturned cars on I-96 near Webberville and Detroit area roads flooded
- A tornado ripped through West Michigan Thursday night, along with a round of thunderstorms causing severe damage and leaving over 240k without power
- The storm, with wind gusts reaching over 85 mph, overturned cars, downed trees, flooded towns and destroyed buildings and homes
- Injuries have been reported in Kent County. A woman and two children were killed in a hydroplaning crash, according to Fox17
Read the original article by clicking here.

Important Takeaways:
- Train derails outside Detroit, Michigan, with one car carrying hazardous materials
- Van Buren Township train derailment unfolds nearly two weeks after East Palestine, Ohio disaster
- A train containing one car of hazardous materials has derailed Thursday in Van Buren Township outside Detroit, Michigan, reports say.
- The cause of the derailment was not immediately clear.
- Police told Fox2 Detroit that there were no injuries and the area is not a hazmat situation.
- Officials that spoke to WXYZ, which reported that at least six cars were seen off the track, said one of them was carrying hazardous materials.
Read the original article by clicking here.

Mark 13:12 “Brother will betray brother to death, and a father his child. Children will rebel against their parents and have them put to death.
Important Takeaways:
- Michigan State shooter who killed 3 students, injured 5 identified as Anthony McRae
- Campus police say two people were killed at Berkey Hall and another was killed at the MSU Union, while five people were in critical condition at Sparrow Hospital. The shooter eventually killed himself, police announced early Tuesday.
- The gunfire began around 8:18 p.m., inside Berkey Hall on the northern boundary of campus, prompting the school to send out a shelter-in-place order at 8:31 p.m.
- After shots were fired inside Berkey Hall, the suspect walked to the MSU Union and opened fire, police said.
- Michigan State University Police Deputy Chief Chris Rozman told reporters Tuesday that “We have absolutely no idea what the motive was at this point” for the mass shooting
- We can confirm that the 43-year-old suspect had no affiliation to the university,” he said. “He was not a student, faculty, staff, current or previous.”
- So that’s an unknown right now. And that’s what we’re trying to understand is why this incident occurred,” Rozman added. “I know everybody wants to know what the motive is. We don’t have an answer right now. And that’s the honest truth.”
Read the original article by clicking here.
Romans 13:1 says, “Let everyone be subject to the governing authorities, for there is no authority except that which God has established. The authorities that exist have been established by God.”
Important Takeaways:
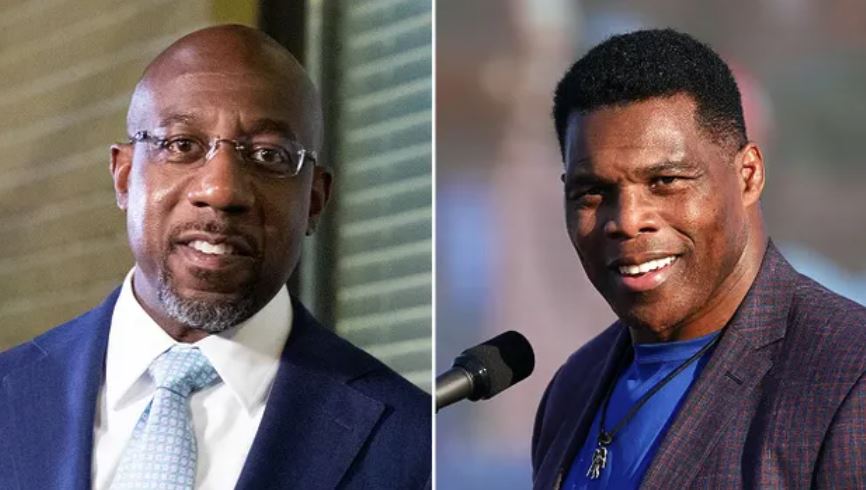
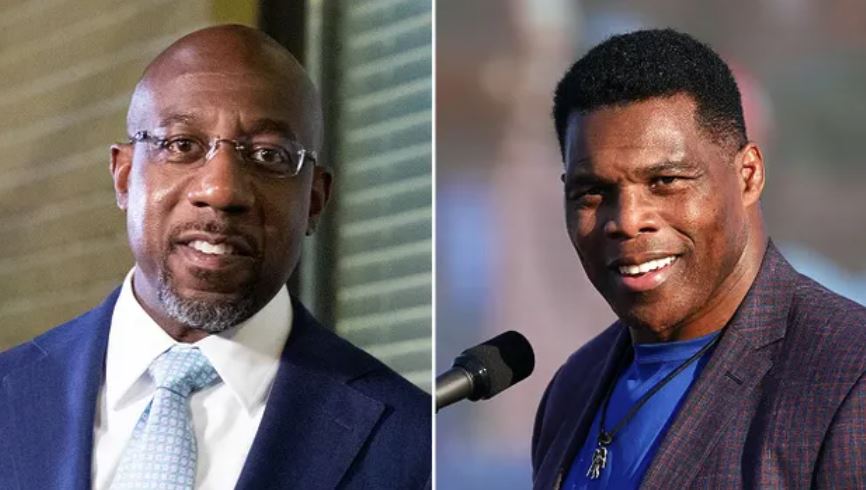
- Georgia’s Senate race still too close, Dow slips, and history has been made in some American states
- Stacey Abrams conceded to Republican challenger Brian Kemp in Georgia
- Gretchen Whitmer defeats Tudor Dixon in Michigan
- Republican George Santos flipped the 3rd Congressional district in New York
- 4 Senate seats are still up for grabs: Nevada, Georgia, Wisconsin and Arizona. Delay in Arizona’s Maricopa County due to “ballot glitches” and additional results are expected on Wednesday night.
- Some of the top issues for American voters during this election cycle included inflation, threats to democracy, crime, immigration and border security, and abortion.
Read the original article by clicking here.